Cauda Equina Syndrome Definition & Function
|
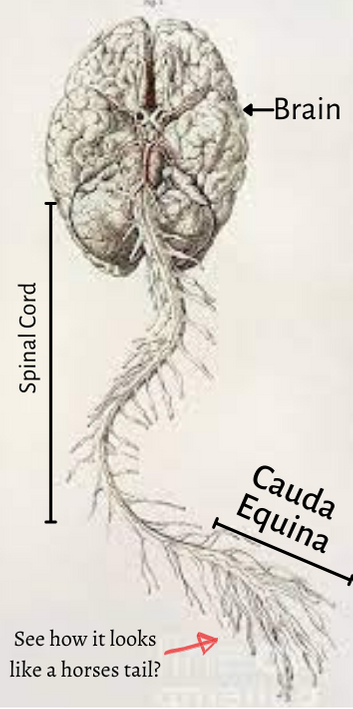
Cauda Equina Syndrome is a rare spinal disorder that causes a collection of neurological and systematic symptoms due to an injury to the spinal nerve roots called the cauda equina (CE). The cauda equina is located in the lumbar spinal canal and down through the sacrum. Cauda equina translates from latin to mean "horses tail" as that was how it was described during dissection of a cadaver.
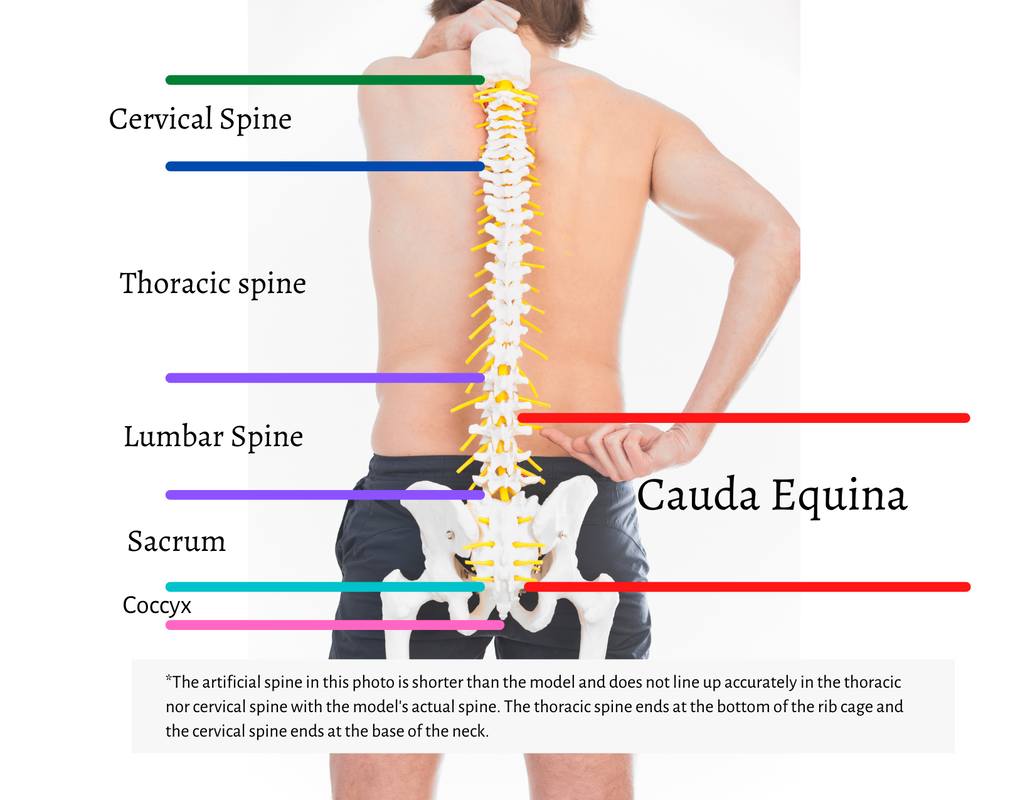
The cauda equina transmits signals to the lower body from the spinal cord and from the lower body to the spinal cord; it is the relay center of motor and sensory signals both to and from the lower extremities, genitalia, lower abdomen, bladder, and bowels. Anatomy- VertebraTo understand the cauda equina it is helpful to know the anatomy of the spine. The spine begins at the base of the skull and is broken up into five segments- cervical, thoracic, lumbar, sacral, and coccyx- each segment is supported by boney structures called vertebrae.
Vertebrae are labeled by the segment type followed by the number of the level from the skull down. For instance, the first level of the cervical vertebrae is C-1. There are seven/7 levels in the cervical segment labeled as C-1 thru C-7. There are 12 thoracic vertebrae labeled T1 thru T12, there are five lumbar vertebrae labeled L1 thru L5. The sacrum is labeled as S1 thru S5, however in a person's mid thru late 20's the sacrum becomes fully fused into one segment and is generally not labeled as individual segments after that time. The tailbone, or coccyx is made up of 3 o 5 bones- it differs from person to person and is no longer necessary to the function of the spinal column. When talking about an intervertebral disk injury level, two levels are affected when one area is injured- more on that later. So to label an intervertebral disk injury both the level above the injury and the level below the injury are named. For example, the lumbar spine intervertebral di L1-L2 or L4-L5, or L2-L5 if it is multiple levels of injury. The same holds true for the cervical and thoracic intervertebral disk injuries. There are exceptions to this rule- such as when the injury is specific to an vertebrae. When speaking of an injury to the boney structures, it would be labeled as the segment and then the number of the vertebrae starting from the top down. For example, if someone fell and broke their fifth thoracic vertebrae the injury would be labeled as injury to the T5 vertebrae. The vertebrae is made up of a body, pedicle, lamina, facet joints, and foramen. |
Cervical SpineThe cervical spine is at the top of the spine starting just below the skull. It functions to support the head and neck, supply nerve function to the face, arms, hands, and upper torso, and to protect the spinal cord. It is made up of 7 bones called the cervical vertebrae.
thoracic is T-x, lumbar is L-x, sacral is S-x, coccyx is not labeled as such, though it does have )followed by the number in which is shows up counting down from the base of the skull. For example the lumbar vertebrae that sits just above the sacrum would be labeled The cervical spine is at the top of the spine starting just below the skull. It functions to support the head and neck, supply nerve function to the face, arms, hands, and upper torso, and to protect the spinal cord. It is made up of 7 bones called the cervical vertebrae. The spinal cord runs from the base of the skull through the cervical spine. Nerve roots exit the spinal canal below the level of bone. In other-words, a C5 nerve root exits in between C5 and C6. |
Cauda Equina Syndrome Stages and categories
The three stages of cauda equina syndrome
There are three stages of Cauda Equina Syndrome; High Risk CES (HR-CES), Acute CES (A-CES), and Chronic Cauda Equina Syndrome (Ch-CES). High risk means that conditions are such that there is a high likelihood of a patient developing A-CES, but they do not currently have A-CES. A-CES is a medical emergency in which patients should proceed to the nearest emergency department for evaluation and treatment. A-CES means that the injury is in progress, it is happening now and for the best possible patient outcome, diagnosis and treatment should be made as soon as possible. The current recommendation for treatment is for it to be completed before 24 hours after the ONSET of CES symptoms started (this may be different for individuals with slow onset CES, but that is discussed elsewhere). Patients that were misdiagnosed, or delayed diagnosis or treatment are NOT the same as a slow onset CES patient. A-CES is A-CES whether it is timely diagnosed or not.
Acute Cauda Equina Syndrome
A series of symptoms that arise from acute injury of the cauda equina. This means that the injury has just happened or is currently happening. This stage requires immediate evaluation by emergency medical teams. If you think you have Red Flag Symptoms of Cauda Equina Syndrome, seek emergency evaluation at the nearest emergency room. With timely treatment, Acute Cauda Equina Symptoms can be reversed or worsening can be stopped. Treatment MUST occur in the first 48 hours from ONSET of symptoms for the best patient outcomes. It is important to note that not all causes of Cauda Equina Syndrome have a treatment at this time.
Acute Cauda Equina Syndrome Symptoms
Symptoms of Acute Cauda Equina Syndrome Include:
- bladder and/or bowel dysfunction (incontinence is a late sign and has the poorest prognosis)
- paresthesia and/or anesthesia of the lower extremities, lower abdomen, perineum, and/or genitalia
- sciatica, usually bilateral, but not always
- severe lower back pain
- lower extremity weakness
- abnormal and/or absent reflexes
- foot drop
- hip drop
- gait disturbances and/or inability to walk
- abnormal proprioception
- sexual dysfunction
Causes of Acute Cauda Equina Syndrome include:
- disk herniation (most common)
- tumor
- spinal stroke
- blood clot
- infections (including Tuberculosis)
- meningitis
- traumas
- lumbar surgery
- epidural steroid injections (esi)
- epidurals
- childbirth
- shearing (sudden stretching of the cauda equina)
- tethered cord
- hematomas
- neuroinflammation
- accidental injury during lumbar procedures
- Arachnoiditis
- Adhesive Arachnoiditis
- broken vertebrae
- other unknown causes (given the limited amount of CES research, this list is still growing)
- Cancer
- Chemotherapy
- Radiation
Potential Recovery Stage Cauda Equina Syndrome (PRS CES)
The stage after initial treatment expected recovery time when treatment is possible as not all causes of CES are treatable but before 24 months. This timeframe is the greatest chance of recovery of function and reversal of deficits. (This is not an official stage recognized by medical literature, but is a gray area without a name.)
Chronic Cauda Equina Syndrome
A patient that has been diagnosed with CES and has not made a full recovery in 24 months. These individuals will likely have the symptoms they are experiencing at 24 months for the rest of their lives with periods of flare-ups. These individuals can make small and slow recoveries over many years with proper therapy and treatments.
Chronic Cauda Equina Syndrome Symptoms
Common member reported symptoms of Chronic CES PLUS Neuroinflammation Symptoms and increased risks of other co-morbidities including:
Not every Chronic Cauda Equina Syndrome patient has every symptom listed, however, this is a list of the most common symptoms reported by our members. Many have one side worse than the other, but usually have bilateral symptoms. Rarely will only one side be affected, but it is reported. We are currently involved in a Delphi Study to determine the most important patient outcomes to those with Cauda Equina Syndrome.
- Chronic and Chronic Intractable Pain
- Electric Shocks
- Tremors
- Flare-ups of Neuroinflammation causing increase in symptoms
- Chronic Pain
- Intractable Pain
- Lower Extremity Swelling and Poor Circulation (slowed healing of wounds)
- Poor Temperature Regulation of the Lower Extremities
- Falls and increased risks of fall-related injuries, subsequent hospital admissions, and subsequent surgeries to repair fall-related injuries
- Mental Health Disorders including Depression, Anxiety, and PTSD
- Musculoskeletal Pain from Compensatory Gait Imbalances
- Higher risks of osteoporosis from medication side effects and lack of mobility and weight-bearing
- Obesity and subsequent co-morbidities,
- Higher risks of blood clots and associated risks, pulmonary embolism and stroke
- Higher risks of heart disease
- Higher risks of diabetes
- Changes in bone structure due to joint instability
- Shoulder disorders due to assistive walking devices and wheelchair use
- Increased risks of pressure sores and associated infections
- Chronic Urinary Tract Infections
- Chronic Constipation
- Restless Back Syndrome (Exactly like Restless Leg Syndrome except in the Back and not associated with Secondary Restless Leg Syndrome)
- Pseudodementia “Brain Fog”
- Fatigue
- Sciatica (usually bilateral)
- Radiculopathy
- Neuropathy
- Social Economical Devastation (due to decreased ability to work or complete inability to work)
- Facet Arthropathy
- Facet Hypertrophy
- Spinal Instability
- Failed Back Surgery Syndrome
- Arachnoiditis
- Bladder Dysfunction
- Bowel dysfunction
- Paresthesia and/or anesthesia of the lower extremities and genitalia
- *Severe Lower Back Pain
- Lower extremity weakness
- Abnormal or absent reflexes
- Foot drop (can be unilateral or bilateral)
- Hip drop
- Gait Disturbances,
- Abnormal Proprioception
- Sexual Dysfunction
- Adhesive Arachnoiditis
- Spasticity (Food for thought. CES is a peripheral nervous system injury, spasticity should not be possible, other than in the bladder. We know the cauda equina is not a central nervous system disorder, and therefore not a spinal cord injury because the cauda equina is made up of lower motor neurons. Does this mean that the cauda equina has its own characteristics different from peripheral nerves outside of the spinal column? We don’t know, research is needed.)
Not every Chronic Cauda Equina Syndrome patient has every symptom listed, however, this is a list of the most common symptoms reported by our members. Many have one side worse than the other, but usually have bilateral symptoms. Rarely will only one side be affected, but it is reported. We are currently involved in a Delphi Study to determine the most important patient outcomes to those with Cauda Equina Syndrome.
Cauda Equina Syndrome Severity Classifications
In addition to Acute, PRS, and Chronic Cauda Equina Syndrome, there are classifications of severity of Cauda Equina Syndrome, currently in literature Incomplete Cauda Equina Syndrome (CES-I) and Complete Cauda Equina Syndrome (CES-C). Some literature, particularly outside of the United States, classify CES-C as CES-R or retention, for the purpose of our education we will use CES-R for High-Risk Cauda Euqina Syndrome.
High-Risk Cauda Equina Syndrome
High-Risk Cauda Equina Syndrome, CES-R, is a classification for individuals showing mild RED Flag Symptoms of Cauda Equina Syndrome but do not have evidence of emergent need for surgery or treatment on imaging, nor are they officially diagnosed with Cauda Equina Syndrome. These patient require close monitoring, education, and a treatment plan.
CES-R patients may have more conservative treatments including physical therapy, pain management, inflammation treatment, and very close monitoring. When the cause of CES-R is a mechanical reason, something that can be fixed surgically, some physicians will choose to proceed with surgical repair to prevent Cauda Equina Syndrome. It is important to note that individuals that have CES-R can transition to Incomplete or Complete Cauda Equina Syndrome at any moment, depending on what is causing the symptoms. There have been patient reported cases of transitioning from CES-R to CES-I from sneezing, vacuuming, tripping, falling, and "waking up with it". Patient education is extremely important for patients that are on a conservative treatment plan, particularly when to return to the emergency department and activities to avoid.
23-hour observation, neurosurgery consult, pain management, fall precautions, spinal precautions, blood clot prevention, patient education, pressure sore prevention (remember these patients might have decreased mobility and sensation). The neurosurgeon will make further recommendations and more in-depth treatment plan.
The definition of CES-I, in literature, is Cauda Equina Syndrome in which an individual is NOT incontinent. These individuals may or may not have bladder dysfunction, urinary retention, urinary leakage, and trouble initiating and maintaining flow, they may even need to catheterize at times, and have chronic urinary tract infections, however, they are NOT incontinent. Unfortunately, this same individual can have every other issue listed above in the Chronic CES list but because they are not incontinent they are not considered complete for severity scoring.
Complete CES is defined as individuals with CES that have incontinence. These individuals may also have every symptoms off of the Chronic CES list, however, even when they only have incontinence (as horrible as that is) they are not as severe as someone with CES-I that also has many symptoms on the Chronic CES list of symptoms. For this reason, Cauda Equina Foundation is working to develop a better scoring system. In some countries, the CES-I or CES-C classification determines eligibility for services and assistance and with the current scoring system, this is a major disservice to those individuals with catastrophic CES that are still considered incomplete.
Perhaps additional scoring will include catastrophic CES in which individuals that have “x” number of devastating symptoms are classified? Only research will tell.
CES-R patients may have more conservative treatments including physical therapy, pain management, inflammation treatment, and very close monitoring. When the cause of CES-R is a mechanical reason, something that can be fixed surgically, some physicians will choose to proceed with surgical repair to prevent Cauda Equina Syndrome. It is important to note that individuals that have CES-R can transition to Incomplete or Complete Cauda Equina Syndrome at any moment, depending on what is causing the symptoms. There have been patient reported cases of transitioning from CES-R to CES-I from sneezing, vacuuming, tripping, falling, and "waking up with it". Patient education is extremely important for patients that are on a conservative treatment plan, particularly when to return to the emergency department and activities to avoid.
23-hour observation, neurosurgery consult, pain management, fall precautions, spinal precautions, blood clot prevention, patient education, pressure sore prevention (remember these patients might have decreased mobility and sensation). The neurosurgeon will make further recommendations and more in-depth treatment plan.
The definition of CES-I, in literature, is Cauda Equina Syndrome in which an individual is NOT incontinent. These individuals may or may not have bladder dysfunction, urinary retention, urinary leakage, and trouble initiating and maintaining flow, they may even need to catheterize at times, and have chronic urinary tract infections, however, they are NOT incontinent. Unfortunately, this same individual can have every other issue listed above in the Chronic CES list but because they are not incontinent they are not considered complete for severity scoring.
Complete CES is defined as individuals with CES that have incontinence. These individuals may also have every symptoms off of the Chronic CES list, however, even when they only have incontinence (as horrible as that is) they are not as severe as someone with CES-I that also has many symptoms on the Chronic CES list of symptoms. For this reason, Cauda Equina Foundation is working to develop a better scoring system. In some countries, the CES-I or CES-C classification determines eligibility for services and assistance and with the current scoring system, this is a major disservice to those individuals with catastrophic CES that are still considered incomplete.
Perhaps additional scoring will include catastrophic CES in which individuals that have “x” number of devastating symptoms are classified? Only research will tell.
|
Vertical Divider
|
Acute Cauda Equina Syndrome-
EMERGENCY Definition
Acute Cauda Equina Syndrome (CES) is a medical emergency in which there is pathology currently causing damage to the cauda equina. Acute Cauda Equina Syndrome requires emergency evaluation, timely diagnosis, and emergent treatment to reverse and/or stop the worsening of the symptoms of Cauda Equina Syndrome.
i. Red Flag symptoms include:
Other patient-reported symptoms to be aware of in assessing risks and likelihood of Cauda Equina Syndrome. Note: These symptoms are commonly reported by members of Cauda Equina Foundation but are not yet well studied or reported in patient outcomes. These symptoms have been reported by both Acute and Chronic Cauda Equina Syndrome patients.
|
Initial Recovery After Acute Cauda Equina Syndrome:
This phase is post-treatment-diagnosis of Cauda Equina Syndrome. The initial recovery stage is where there is a need for the most support and education for the patient and their families. Cauda Equina Syndrome is a family diagnosis, and as such, can change family dynamics and social-economical status. Patients needs can include physical and occupational therapy evaluations and plans, pain management, assistive devices/technology assessments and education, functional wheelchair assessment and fittings, social work and services consults, possible home evaluations (ramps, widening of doorways), driving accommodations and evaluations, transportation accommodations, both patient and family counseling, and food assistance. It is imperative to send patients newly diagnosed with Cauda Equina Syndrome home with a plan for healing, recovery, and guidance to independence.
Patients with newly diagnosed Cauda Equina Syndrome may need complete care initially. They will be limited in their ability and on physicians directions to not lift, bend, twist, or do most household chores nor strenuous activity. They may also not be cleared to return to work for several weeks to months. Depending on their occupation, they may need to change occupations. Some individuals are not able to return to working status due to the severity of their symptoms and lack of recovery.
It is important to understand that Cauda Equina Syndrome is a chronic illness, NOT a bad back. A syndrome is a collection of symptoms making up an illness. The surgery and initial treatments may prevent further damage, with the goal of completely reversing the damage in all patients. At the current time, many individuals do not fully recover physically. It is certainly okay to encourage individuals towards independence, however, it is equally important to understand that the individuals may need help in learning how to live and function again. They must have a support system that is able to help them with their limitations. Many individuals, even those with full recovery, are restricted from certain actions for the rest of their lives. Such actions are repetitive movements, like sweeping and vaccuming, lifting over 10lbs, and high impact activites, such as running and jumping. The physician is the best person to talk to about any physical restrictions placed on an individual. They may have to adapt how they used to do things, such as laundry, grocery shopping, and cooking. Please understand that the families expectations of recovery must be realistic to aid healing of the individual. Expected recovery is explained below.
Recovery is greatest in the first 18-24 months after initial diagnosis. However, small, slow improvements can still be made after the 24 months. The first several months following treatment for cauda equina syndrome are the most intense as far as individuals reliance on others for basic necessities in life, such as eating, bathing, and dressing. These are called activieties of daily living (ADL). Physical and occupational therapy can help individuals gain their independance in their ADL's, however, it is improtant to understand that not all individuals will recover full independence. Some individuals become fully independent with adaptations and accessible equipment, others cannot. Those that do not will need help with adapting ADL's to fit their limitations, and may need permanent caregivers to help them throughout their lives.
Patients with newly diagnosed Cauda Equina Syndrome may need complete care initially. They will be limited in their ability and on physicians directions to not lift, bend, twist, or do most household chores nor strenuous activity. They may also not be cleared to return to work for several weeks to months. Depending on their occupation, they may need to change occupations. Some individuals are not able to return to working status due to the severity of their symptoms and lack of recovery.
It is important to understand that Cauda Equina Syndrome is a chronic illness, NOT a bad back. A syndrome is a collection of symptoms making up an illness. The surgery and initial treatments may prevent further damage, with the goal of completely reversing the damage in all patients. At the current time, many individuals do not fully recover physically. It is certainly okay to encourage individuals towards independence, however, it is equally important to understand that the individuals may need help in learning how to live and function again. They must have a support system that is able to help them with their limitations. Many individuals, even those with full recovery, are restricted from certain actions for the rest of their lives. Such actions are repetitive movements, like sweeping and vaccuming, lifting over 10lbs, and high impact activites, such as running and jumping. The physician is the best person to talk to about any physical restrictions placed on an individual. They may have to adapt how they used to do things, such as laundry, grocery shopping, and cooking. Please understand that the families expectations of recovery must be realistic to aid healing of the individual. Expected recovery is explained below.
Recovery is greatest in the first 18-24 months after initial diagnosis. However, small, slow improvements can still be made after the 24 months. The first several months following treatment for cauda equina syndrome are the most intense as far as individuals reliance on others for basic necessities in life, such as eating, bathing, and dressing. These are called activieties of daily living (ADL). Physical and occupational therapy can help individuals gain their independance in their ADL's, however, it is improtant to understand that not all individuals will recover full independence. Some individuals become fully independent with adaptations and accessible equipment, others cannot. Those that do not will need help with adapting ADL's to fit their limitations, and may need permanent caregivers to help them throughout their lives.
Prognosis:
Prognosis is almost impossible to determine before the first 18-24 months, due to the inflammatory process of healing. However, the prognosis is determinant on the severity of the injury, slow onset vs. sudden onset, classification of cauda equina syndrome at the time of diagnosis, surgical technique, time from onset of symptoms to treatment, and other factors not yet understood. Patients that do not have Complete Cauda Equina Syndrome, and have treatment in under 48 hours of onset of symptoms have the best prognosis for full recovery. Patient outcomes are currently under investigation.
After the patient’s symptoms of cauda equina remain unchanged for a period of time or do not fully resolve after 24 months. They are then classified as having Chronic Cauda Equina Syndrome.
It is important to note that not all patients end up with Chronic Cauda Equina Syndrome, but those that do are not expected to return to their pre-CES selves, though they can make slow improvements with proper care over time.
It is important to note that not all patients end up with Chronic Cauda Equina Syndrome, but those that do are not expected to return to their pre-CES selves, though they can make slow improvements with proper care over time.
ii.Pathophysiology (What happens)
iii.Etiology (Causes)
a. Herniated disk (most common)
b. Tumors
c. Epidurals
d. Trauma- falls, accidents, gunshot wounds, stabbings
e. Shearing (sudden stretching of the cauda equina)
f. Tethered Cord
g. Infections of the cerebral spinal fluid
h. Spinal Stroke
i. Hematomas
j. Neuroinflammation
k. Epidural Steroid Injections
l. Accidental injury during procedures or surgeries of the lumbar spine
M. Arachnoiditis and Adhesive Arachnoiditis
N. Child Birth
O. Broken vertebrae
P. Tuberculosis and other infections
Q. Infections of the cerebral spinal fluid
R. Spinal Taps
R. and other unknown causes
b. Tumors
c. Epidurals
d. Trauma- falls, accidents, gunshot wounds, stabbings
e. Shearing (sudden stretching of the cauda equina)
f. Tethered Cord
g. Infections of the cerebral spinal fluid
h. Spinal Stroke
i. Hematomas
j. Neuroinflammation
k. Epidural Steroid Injections
l. Accidental injury during procedures or surgeries of the lumbar spine
M. Arachnoiditis and Adhesive Arachnoiditis
N. Child Birth
O. Broken vertebrae
P. Tuberculosis and other infections
Q. Infections of the cerebral spinal fluid
R. Spinal Taps
R. and other unknown causes
v.Diagnosis/Testing
- Magnetic Resonance Imaging (MRI)- is the “gold standard” of diagnosis of cauda equina syndrome
- Computerized Tomography (CT)/Computerized Axial Tomography (CAT scan)- Can be used to rule out cases of cauda equina syndrome when MRI is not available. However, it is important to note that it is not diagnostically definitive as CT images can miss images of nerve compression or infraction.
- Myelography- This procedure is used to detect spinal cord injury and to view the nerve roots under contrast. It is not recommended as the first diagnostic tool as it requires the induction of contrast into the spinal column and can cause cauda equina syndrome in rare cases.
- X-ray- This is not recommended to rule out cauda equina syndrome as it will not show soft tissue damage or disk herniation. This procedure is recommended as an additional test to the MRI to view bone structures.
- Time to decompression surgery is one of the most important factors to a positive prognosis, though there are other factors at play. Some studies suggest that the prognosis is determined by the severity of the injury within the first six hours of injury. Remember, the fastest way to a proper diagnosis is through a thorough physical exam, recognizing the Red Flag symptoms, and MRI, the gold standard to diagnosis. Remember not all causes of CES are fixed surgically, such as CES resulting from epidurals. In such cases where injury is not caused by an anatomical structure, such as herniated disk or tumor, injury may not show up on MRI and may require myelography to determine injury.
- Nerve Conduction Study(NCS)- measures how fast and how efficient a nerve can carry a signal. This test is used to determine which nerves are affected, how severely, and their rate of healing over time. It is not recommended to use this test as a diagnostic tool to rule out CES as it is not specific to the cauda equina. However, it is useful post diagnosis and after corrective surgery to establish a baseline of nerve function.
- Electromyogram (EMG)- measures the electrical activity of the muscles both at rest and during to contraction. This test determines how well the muscles are functioning and the severity of potential muscle weakness. It is not recommended to use this test as a diagnostic tool to rule out CES as it is not specific to the cauda equina. However, it is useful post diagnosis and after corrective surgery to establish a baseline of nerve function.
vi.Classifications
1.There are three recognized classifications of Cauda Equina Syndrome:
a.CES-R: Risk of Cauda Equina Syndrome, also referred to as pre-clinical. These patients may have radiculopathy, bi-lateral sciatica, and some changes in sensation in the saddle region and/or lower extremities, however, there are no bladder or bowel disturbances, sexual function is normal, and may not show any significant compression of the cauda equina. These individuals may have large herniations that are not yet completely compressing the cauda equina but are causing neuroinflammation of the arachnoid layer causing inflammation to the cauda equina.
b.CES-I: Incomplete Cauda Equina Syndrome, which is classified as individuals with known or unknown insult/trauma to the cauda equina, but are not incontinent. They may have neurogenic bladder, or urinary hesitancy and/or leakage/accidents. There are further classifications of severity in Incomplete Cauda Equina Syndrome:
a.CES-R: Risk of Cauda Equina Syndrome, also referred to as pre-clinical. These patients may have radiculopathy, bi-lateral sciatica, and some changes in sensation in the saddle region and/or lower extremities, however, there are no bladder or bowel disturbances, sexual function is normal, and may not show any significant compression of the cauda equina. These individuals may have large herniations that are not yet completely compressing the cauda equina but are causing neuroinflammation of the arachnoid layer causing inflammation to the cauda equina.
b.CES-I: Incomplete Cauda Equina Syndrome, which is classified as individuals with known or unknown insult/trauma to the cauda equina, but are not incontinent. They may have neurogenic bladder, or urinary hesitancy and/or leakage/accidents. There are further classifications of severity in Incomplete Cauda Equina Syndrome:
- Mild: Sensory or Motor deficits resulting from acute cauda equina syndrome without bladder, bowel, and sexual dysfunction.
- Moderate: Sensory and/or Motor deficits with some bladder and bowel control deficits such as, frequent constipation, and incomplete emptying of the bladder. Additionally, there are changes in sexual function, but the individual is still able to participate in sexual relationships.
- Severe: Sensory and Motor deficits with minimal bladder and bowel function, and minimal or no sexual function. CES-C is impending at this stage.
vii.Treatment
1.Cauda Equina Syndrome caused by structural anomalies such as herniated disk, tumors, or fractures, require emergency surgery within 48 hours of onset of symptoms to decompress the cauda equina. Current literature suggests that the sooner the surgery the more likely
viii.Post Surgical Care
- Physical Therapy
- Occupational Therapy
- Bladder Care
- Bowel Care
- Pain Management
ix.Post Surgical Home Care
- Physical Therapy
- Occupational Therapy
- Bladder Care
- Bowel Care
- Pain Management
- Caregiver Education
What are the symptoms?
Cauda Equina Foundation's vision is to eradicate the devastating neurological deficits caused by Cauda Equina Syndrome.
Who does it affect?
Cauda Equina Foundation's current strategic focus for 2016-2017:
Who does it affect?
How is it treated?
Cauda Equina Foundation's vision is to eradicate the devastating neurological deficits caused by Cauda Equina Syndrome.
Who does it affect?
Cauda Equina Foundation's current strategic focus for 2016-2017:
Who does it affect?
How is it treated?
Education Initiatives:
Research Initiatives:
Epidemiology: Who is CES affecting and what are those effects? How prevalent is CES? What is the impact of CES on society?
Clinical Practice Guidelines: We are researching peer reviewed retrospective case studies of CES to make evidence based clinical practice guidelines for the timely diagnosis of CES.
Advocacy:
Healthcare Practitioners: We are educating the medical community to improve the quality of care CES individuals receive.
Community: We are educating the community on CES to improve awareness and empathy for individuals living with CES.
Government: We are writting our local, state, and federal legislaters to educate them on the effects of CES, in hopes to streamline and improve the approval rates for disability payments.
- Continuing education programs for healthcare practitioners.
- Case study review for allied health practitioner students.
- CES information library for educational resources.
- Brochures for patients, caregivers, and the community.
Research Initiatives:
Epidemiology: Who is CES affecting and what are those effects? How prevalent is CES? What is the impact of CES on society?
Clinical Practice Guidelines: We are researching peer reviewed retrospective case studies of CES to make evidence based clinical practice guidelines for the timely diagnosis of CES.
Advocacy:
Healthcare Practitioners: We are educating the medical community to improve the quality of care CES individuals receive.
Community: We are educating the community on CES to improve awareness and empathy for individuals living with CES.
Government: We are writting our local, state, and federal legislaters to educate them on the effects of CES, in hopes to streamline and improve the approval rates for disability payments.
Refrences:
1. Gofur EM, Singh P. Anatomy, Back, Vertebral Canal Blood Supply. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541083/. Accessed October, 14, 2021.