|
By Dr. Heather Rader, PT, DPT, PRPC, BCB-PMD Pelvic Physical Therapist and Medical Board Member of the Cauda Equina Foundation Just like in medicine, physical therapy has different specialties. A pelvic physical therapist has extra training to treat the muscles in the perineum and pelvic floor region of the body. These muscles give you bowel and bladder control and assist in sexual functions. Using exercise prescription, manual therapy, and modalities such as electrical stimulation and biofeedback, pelvic P.T.’s treat problems such as incontinence, constipation, painful sex, and sitting pain.
If your CES gives you any of the following symptoms, then a pelvic health physical therapist should be a part of your healthcare team. Bladder Symptoms • Urinary urgency – a strong, sudden urge to urinate, often with very little urine output • Urinary frequency – going too often – more than 8 times a day, or less than every 2 hours • Nocturia – waking up 2 times or more a night to urinate • Decreased awareness of bladder fullness • Effortful urination – straining to start or maintain the urine flow • Feeling the bladder is incompletely emptied after going • Stress Urinary incontinence – leakage with a cough or sneeze, while lifting things, or when exercising • Urge Urinary incontinence – leakage during an urge to go or not making it in time • Overactive Bladder – a bladder syndrome that includes urgency, frequency, nocturia, and/or incontinence • Pain in the lower abdomen as the bladder gets full • Pain in the urethra as urine comes out • Self-catheterization support Bowel Symptoms • Constipation – slow transit type with BM’s occurring 2 times a week or less • Constipation – outlet obstruction due to overactive pelvic floor muscles or prolapse • Fecal urgency – strong, sudden urges to have a BM • Fecal frequency – routinely going 4 times or more a day • Fecal incontinence – from fecal smearing on undergarments to loss of entire bowel contents • Effortful BM’s – excessive straining to go or taking longer than 5-10 minutes to complete a BM • Painful BM’s – abdominal or pelvic pain as the bowels fill up or pain during a BM Sexual or Reproductive Health • Pain during sex at the vaginal opening or deep in the pelvis • Pain during sex in the scrotum or penis during erection or ejaculation • Changes in orgasm – unable to achieve, takes a long time, or lowered intensity • Dysmenorrhea – extremely painful menstruation • Abdominopelvic pain syndromes like endometriosis • Vulvar and vaginal pain syndromes • Prostate related pain syndromes Where can I find a pelvic PT? Here are some national locator links. You can also do a Google search in your local area by using some of the following keywords and combinations: Pelvic Floor, Pelvic Health, Pelvic Physical Therapist near me. • PelvicRehab.com • APTAPelvicHealth.org/PTLocator • PelvicGuru.com Regardless of how long you have had symptoms, a pelvic physical therapist can still help you minimize bowel and bladder symptoms and help reduce your pelvic pain. Talk to your doctor about it. Reach out to the therapist directly. Most states do not require a doctor’s order to get started with treatment. Don’t assume you are stuck with the symptoms of CES – Find a Pelvic PT today!
0 Comments
As a registered nurse who also has been affected by Cauda Equina Syndrome (CES), I have many of the same concerns that we all have during the current COVID pandemic and influenza season. As individuals living with CES, regular handwashing is the best way to remove germs, avoid getting sick, and prevent the spread of germs to others (Centers for Disease Control and Prevention, 2021). Washing your hands often, especially when we are likely to get and spread germs, is the most critical measure to help prevent COVID and other usual germs (Haston et al., 2020).
A US Adult internet survey showed that one out of four people does not wash their hands after coughing, sneezing, or blowing their noses. Fewer than 75% of respondents reported remembering to wash their hands after having respiratory virus symptoms or eating. Research shows that men, young adults ages 18 to 24 years old, and white adults are less likely to remember to wash their hands regularly (Haston et al., 2020). Alcohol-based hand sanitizer is preferred over soap and water in most situations due to the fact that it is readily available (Centers for Disease Control and Prevention, 2020a). Alcohol-based hand sanitizer kills most of the harmful germs and does not create antibiotic-resistant superbugs (Centers for Disease Control and Prevention, 2020b). The CDC recommends these critical situations where we should clean our hands, either with alcohol-based hand sanitizer or soap and water (Centers for Disease Control and Prevention, 2020b):
Cauda Equina Syndrome can cause us to have frequent urinary tract infections. The involved nerves may affect the bladder, bowel, and genital areas, and many of us require regular invasive procedures for this reason (Wiseman, 2021). Before completing any urinary or bowel tasks, such as straight catheterization or a bowel program, hand washing or using an alcohol-based hand sanitizer should be completed. Handwashing with soap and water should be done after the task, as hand sanitizer does not kill the germs that cause severe diarrhea (Centers for Disease Control and Prevention, 2020b). Please, stay safe, perform regular hand washing or sanitizing, and “Speak Up for Clean Hands” to remind those around you to do the same (Centers for Disease Control and Prevention, 2020b). References Centers for Disease Control and Prevention. (2020a, February 13). Hand hygiene guidance | hand hygiene | cdc. https://www.cdc.gov/handhygiene/providers/guideline.html Centers for Disease Control and Prevention. (2020b, February 13). Patients | hand hygiene | cdc. https://www.cdc.gov/handhygiene/patients/index.html Centers for Disease Control and Prevention. (2021, October 15). Handwashing - clean hands save lives | cdc. https://www.cdc.gov/handwashing/index.html Haston, J. C., Miller, G. F., Berendes, D., Andújar, A., Marshall, B., Cope, J., Hunter, C. M., Robinson, B. M., Hill, V. R., & Garcia-Williams, A. G. (2020). Characteristics associated with adults remembering to wash hands in multiple situations before and during the covid-19 pandemic — United States, October 2019 and June 2020. MMWR. Morbidity and Mortality Weekly Report, 69(40), 1443–1449. https://doi.org/10.15585/mmwr.mm6940a2 Wiseman, D. (2021). Cauda equina syndrome – symptoms, causes, diagnosis and treatments. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome
The first things I want to say to you are:
So, What now?How do you fight something that you may not be able to spell or are unsure of how to pronounce, yet- something I had to learn. I've also learned that many of my healthcare providers can't pronounce it either, I correct them and educate them. So, how do you say Cauda Equina Syndrome? Cod-a E-qw-eye-nah Sin-drum Things I wanted to know first. Will I recover? By how much? What do I have to do to recover? Who do I need to see? How do I shower? How do I use the bathroom? How do I get my socks on? How do I pick up the grabber stick that picks stuff up for me that I dropped on the floor (see above picture- why yes, that really is me taking a picture of life's irony)? And a million other things going through your mind. Slow down. Breathe. We've got your back (pun intended). Will you recover? I wish I could tell you unequivocally, Yes! But, the reality is no one knows, not me, not the Foundation, not your fellow CES Warriors, and not your doctors or therapists. It's all probabilities based on a lot of factors and it sucks to not know or have the answers to your questions, believe me, I know, I've been there. But look on the bright side, at this stage, recovery IS a possibility. It takes time and it's slow and frustrating at times, but, at this stage in your diagnosis anything is possible. I remember this one day, I was doing my therapy at home. The occupational therapist had given me a shoebox with rice in it to write the alphabet in with my feet. This was supposed to help me move my feet again and build sensory back. I got good with the motion part except flexing my feet and the sensory not so much, but that is not the point of this story. What is the point is one day I got so frustrated that I couldn't hardly move my foot and I couldn't feel the stupid rice that I kicked the box! Picture this, you're my husband, you're in the other room and you hear &$*@! and a loud crash noise. He comes running into the bedroom to see that I have kicked a shoebox of rice all over the carpet in our bedroom. Now, to truly understand this situation, what you have to know is that at this point he had been waiting on me hand and foot for a month. I was still not able to walk around at the time- I was fully dependent on him to do everything. I was no longer working, I was no longer doing the household shopping, cooking, cleaning, or taking care of the animals. He had to take on everything by himself including taking care of me, while still working full time- from home because I needed 24/7 care. Needless to say, he was not having the best day. I quickly realized that I was not going to be the one that had to clean up the rice, then I started crying my eyes out- so now he's dealing with an emotional wife on top of everything. To his credit, he didn't even yell about it- actually he didn't say a word about it. He just cleaned it and that was that. Yep, ten years later and we are still married and I constantly come up with new ways to cause chaos in our household. He doesn't come running when he hears a loud crash anymore- well, unless he doesn't hear "I'm okay" yelled out right afterwards that is. The point of me telling you that? Well, if you are the patient reading this, know that you will get frustrated. It's okay, and it's normal. Maybe don't kick a box of rice, but do find an outlet for your frustration. If you are the caregiver, friend, or family member, know that we get frustrated because our body doesn't work right and we have lost our independence- having you there to support us and clean our messes is the best thing you can do for us. Also know that you are allowed to get frustrated too- find a healthy outlet for your frustration and know that caregiver fatigue is a real thing- take breaks and ask for help! Special Note: There are different stages to cauda equina syndrome- if you are reading this, you have likely already been through the acute stage, or acute cauda equina syndrome (A-CES). A-CES means that the injury to the cauda equina is currently happening and that is why A-CES is a medical emergency- the goal is to stop the injury from getting worse and to try to reverse any damage already done. Generally speaking those with the best outcomes have the least amount of symptoms when they are diagnosed and are treated within 24 hours of the onset of symptoms or from the time of known injury, but there are exceptions to every rule. That is why you will constantly hear, "Maybe", "It's Possible", "I don't know". Yeah, I feel your frustration, I remember it well. This is a marathon, not a race- and that sucks. Just don't forget- NEVER GIVE UP ON YOURSELF! Learn more about here.
Until next time, Amanda Proctor Kicker of Boxes of Rice Director of Chaos CES Fighter! The first few weeks of a Cauda Equina Syndrome Diagnosis
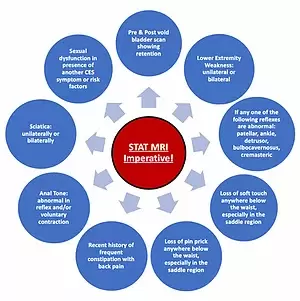
Greetings! If you’re reading this article, I’m guessing you are one of the many searching for more information regarding cauda equina syndrome (CES). You’ve definitely come to the right place! I was diagnosed with CES in December 2015 and it has been quite the journey. I’d like to share with you my experiences during those first weeks and how I was able to stay strong during this time. Like many of you I was misdiagnosed by several medical providers, they missed the CES Red Flags. There is NO consensus on clinical presentation and it may be etiological specific. 3 Many in practice agree that urinary disturbances and saddle anesthesia are the hallmarks of cauda equina syndrome. However, the research does not back this as a Gold Standard. Further t...
This isn’t your fault. More and more administrators and government officials wanting to “improve” healthcare write policies that are out of touch with the reality of direct patient care. They don’t practice physical patient contact and interaction, how can they know ab...
Alone with Cauda Equina Syndrome It has been almost two and a half years since I had surgery for Cauda Equina Syndrome.
I was hurt for nearly a year before I woke up one morning numb from the waist down and wound up in the hospital being prepped for surgery. I was told that I needed a spinal decompression or I would never walk again. I recall discussing my dilemma with the surgeon. |
Archives
June 2022
Categories |




 RSS Feed
RSS Feed