|
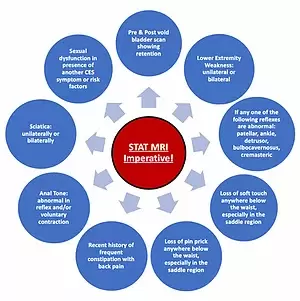
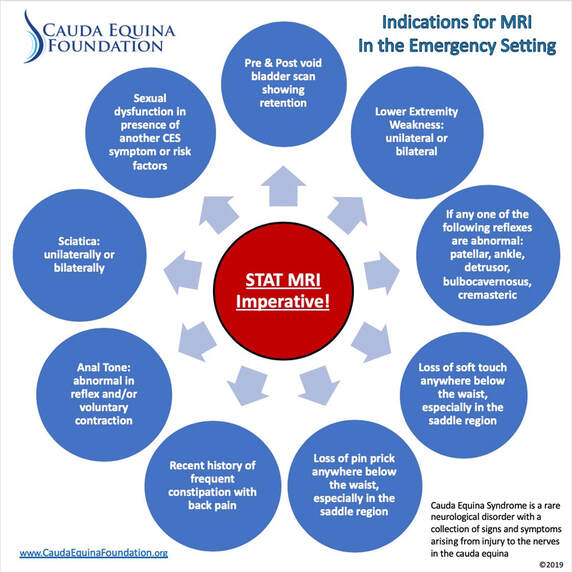
There is NO consensus on clinical presentation and it may be etiological specific. 3 Many in practice agree that urinary disturbances and saddle anesthesia are the hallmarks of cauda equina syndrome. However, the research does not back this as a Gold Standard. Further t... Cauda Equina Foundation Presents: A Clinicians Guide to Cauda Equina Syndrome Definition, Evaluation, and Diagnosis Cauda Equina Syndrome Definition: There is No Consensus of Definition. There are approximately 17 definitions, ranging from etiology specific to pathomechanical, to clinical presentation. 3 Cauda Equina Foundation, Inc. uses a broad definition to encompass all etiologies of cauda equina syndrome. Cauda Equina Syndrome is a rare neurological disorder with a collection of signs and symptoms arising from injury to the nerves in the cauda equina.16 This can lead to confusion in diagnosis upon clinical presentation due to lack of clear definition; leading to high rates of misdiagnosis and misunderstanding of early symptoms.5 Perhaps a consensus of definition should be evaluated to decrease rates of misdiagnosis and delayed care. This proves difficult as clinical presentation can vary upon etiology, proving even more difficult with no consensus on clinical presentation.3,5 Further, there are different types of cauda equina syndrome including rapid onset, slow onset; further divided by incomplete and complete cauda equina syndrome. 5 Rapid onset CES typically follow an event such as trauma or injury; but not always. Further this patient population has poorer outcomes than slow onset CES. 16 There are further inconsistencies in the definitions of compete CES and incomplete CES; while both define neurological bladder deficiencies, some define saddle anesthesia and perineal anesthesia as a factor of classification.16 Incomplete CES (CES-I) is defined here as having urinary deficits including retention, difficulty with flow, and hesitancy.3 Complete cauda equina syndrome (CES-R) is defined here as having urinary retention with overflow incontinence.3 Classification of cauda equina syndrome at time of diagnosis is imperative to determine treatment options. There is no clinical significance in patient outcomes for patients with CES-R to gain benefit postoperatively.4, 9,11, 12,14 The most common cause of misdiagnosis of cauda equina syndrome is failure to consider the diagnosis.5 Clinical Presentation of Cauda Equina Syndrome: There is NO consensus on clinical presentation and it may be etiological specific.3 Many in practice agree that urinary disturbances and saddle anesthesia are the hallmarks of cauda equina syndrome. However, the research does not back this as a Gold Standard. Further there is NO consensus on bladder and saddle sensation involvement.1, 3, 4, 5, 16 Only 19% of patients present with “classic” cauda equina syndrome clinical signs and symptoms. 3 Bladder Presentation: When getting a patient history, it is imperative to know that patients may not realize they have retention. Therefore, asking a patient if they have had bladder disturbances may lead to miscommunication and misdiagnosis and delayed care. Urodynamics can be used as a tool to determine pre and post void volumes to determine presence of retention.16 Absence of bladder or bowel disturbances does not rule out CES.3 Bowel: There is NO consensus for the presence of bowel dysfunction at clinical presentation. Bowel disturbances may be slower onset due to the inability to feel full at time of presentation. However, in slow onset CES, frequent constipation may be a sign of worsening symptoms. 3, 5 Anal Tone: NOT always abnormal.3 Anal tone findings should be assessed for both reflex and voluntary contracture; findings are not correlated with prognosis at this time.3 Pain: There is NO consensus on quality nor location, nor presence of pain for a diagnosis of CES; this may be etiology specific.3 Perhaps in the future with further research pain may be better defined by etiology in CES. Those with pain and sciatica in the lower extremities at the time of clinical presentation have poorer prognosis; both bilaterally and unilaterally. 3 Sensation: There is no consensus on presence or absence of sensation with diagnosis of CES, there is strong agreement.3 25% of patients DO NOT present with saddle anesthesia; those with complete anesthesia have the poorest outcomes.3 The most common sensation deficits were to soft touch and pin prick.3 It is imperative to test the saddle area to both soft touch and pin prick as patients may not realize they have decreased sensation at the time of presentation, particularly if the patient is sudden onset. However, even with slow onset, they may not yet realize the deficit. Power/Strength: There is NO consensus on the relation to strength/power at clinical presentation and diagnosis of CES. Nor is there a correlation with prognosis.3 Just over 50% of patients in one study had lower extremity weakness. 3 Reflexes: There is NO consensus on presence or absence of reflexes in the diagnosis of CES.3 The most important reflexes to evaluate are patellar, ankle, detrusor, bulbocavernosus, and cremasteric.3 Reflex quality and presence or absence have no current correlation between diagnosis and prognosis. Sexual Dysfunction: This is not something that individuals with sudden onset may be aware of and practitioners may not get an accurate assessment. However, individuals presenting with sexual dysfunction in the presence of other CES symptoms, should be evaluated further. Sexual dysfunction may also be the result of other underlying health issues or pharmacological, or psychological in nature. Presence of sexual dysfunction at clinical presentation is not definitive. 3 There are no reports of female sexual dysfunction being evaluated in CES clinical presentation or follow-up care, however, there are sexual dysfunctions that females report post diagnosis, such as vaginal dryness, pain on intercourse, decreased or absent sensation, and incontinence during intercourse. There is no correlation between sexual dysfunction and prognosis at this time. However, it has a significant role in quality of life. To better understand clinical presentation, it would be prudent to conduct a meta analyses and pro forma data collection as well as measure clinical outcomes to better understand prognosis markers. With more research a consensus can be achieved in clinical definition, signs and symptoms at clinical presentation, patient care protocols, and timing to treatment relative to outcomes.3, 5, 11, 15, 16 The most common clinical presentation was pain, and difficulty ambulating. Gait, proprioception, and ataxia are rarely assessed in clinical assessment of CES, but are valuable in detecting early symptoms of CES.16 Risk Factors of Cauda Equina Syndrome:
Epidural Steroid Injections Sciatica Chronic Low Back Pain Recent Child Birth Recent Epidural Lumbar Puncture Fever with neurological changes Recent Ataxia Congenital Disorders Bladder/Bowel Disturbances Sexual Dysfunction Lumbar Surgeries Rheumatoid Arthritis Ankylosing Spondylitis Spinal Stenosis History of Blood Clots Recent Trauma/Injury Neoplastic History Paget’s Disease Arachnoiditis Blood Thinners Degenerative Disk Disease Tarlov Cyst Scoliosis Ehlers-Danlos Syndrome Tuberculosis Spinal Stenosis Diagnosis: Initial signs and symptoms may be subtle and differ amongst etiology.16 Patients with sciatica and low back pain (LBP) should be screened for other less obvious signs and symptoms of CES.16 MRI is the Gold Standard of Diagnosis; however, CT myelogram and CT may be used when MRI is unsafe or unavailable. X-ray will not demonstrate CES. 16 Failure to evaluate urinary retention, bulbocavernosus reflex, saddle anesthesia (soft touch and pin prick) and rectal tone are the most common causes for litigation in the event of misdiagnosis. 16 Urodynamics should be evaluated; in the emergent setting, pre and post void volumes are sufficient. 16 Treatment: Conservative treatment is NOT recommended in a diagnosis of CES with pathomechanical etiology; surgery is an absolute indication in the presence of mechanical causes of CES.15, 16 There is NO consensus on timing of surgery from diagnosis; though there is strong agreement that the surgery should be done as soon as possible; 24-48 hours form onset of symptoms (not from clinical presentation).5, 9, 10, 12, 14,15, 16 Cauda Equina Foundation, Inc. recommends treatment and/or surgery within 24 hours of onset of symptoms based on literature review.14, 15 Cauda Equina Syndrome Prognosis 14, 15, 16:
CES diagnosis is very difficult to recover from, even when treated appropriately. There is no cure, only symptom management. Following a literature review, stakeholder Delphi study, and stakeholder consensus meeting; Patient Outcome Measures of Cauda Equina Syndrome have reached a consensus. Look for publication coming soon. Follow-up research into the process of assessment of outcome measures is in the future. References:
0 Comments
Leave a Reply. |
Archives
June 2022
Categories |

 RSS Feed
RSS Feed